With restful garden spaces, an outdoor gym, pool table and music and art room, the Bluestone Unit is probably not what most people would envisage a mental health inpatient facility to look like.
The unit, based at Craigavon Area Hospital, cares for around 800 patients a year, many of whom feel suicidal and are often grappling with complex problems, from drug and alcohol addiction to eating and perinatal disorders.
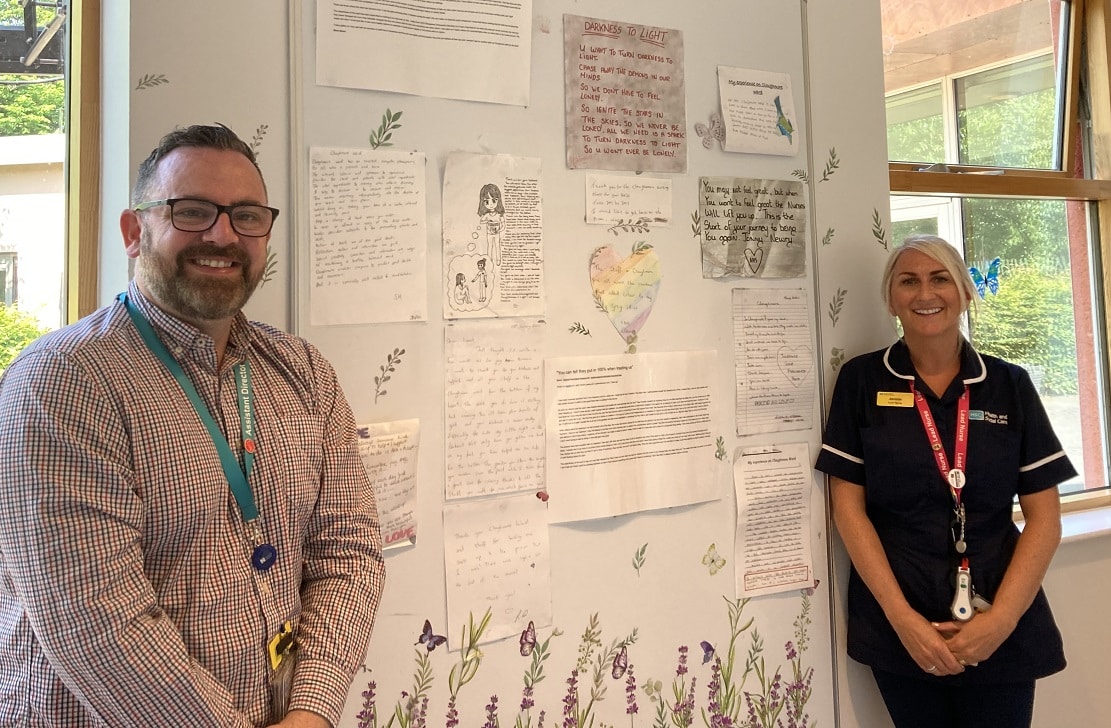
However, as interim assistant director Joe Walker explains, the aim is to rekindle the hope and purpose so many patients have lost and equip them with the skills to deal with any future challenges.
Joe, who worked as a nurse for many years and lives in Armagh, has, along with his team, been spearheading considerable change at the unit over the last 18 months.

A new management structure has been introduced, with a multi-disciplinary team of 204 professionals ranging from consultants and nursing staff to dietetics, podiatry, physiotherapy, speech and language therapy and physicians’ associates.
Meanwhile, the implementation of the tried-and-tested Safewards model puts patients, their families and carers at the centre, by involving them in decisions about everything from meal provision to the types of activities they want, whether that be gardening or arts and crafts.
“We focus on purposeful, meaningful activity provision, with structured sessions across seven days, led by dedicated activity co-ordinators,” says Joe.
“That is so important to recovery. And since introducing structured activities we have also seen a reduction in violence and disruption.”
The unit has 96 beds across seven wards, focusing on general psychiatry, psychiatry of old age, dementia, intellectual (learning) disabilities and psychiatric intensive care.

Discharge letters from patients are attached to display boards in the brightly painted corridors.
One reads: “At the beginning of December 2021, I tried taking my own life. At this time I was very depressed as I had split from my partner and wasn’t able to see my children due to my lifestyle of bingeing on drink and drugs… I lost my job due to these binge cycles and … so having no job led me to money worries so a lot of the stress as well as having no motive in life led me down a dark path which I honestly thought there was no way out of.
“I would not be here if it wasn’t for the support of this service. They have helped me in so many ways and I am so grateful for it.”
Another person who has struggled with their mental health for a long time wrote of the unit: “I always feel valued and cared for and feel safe here.”
Of course, the unit has not been without its criticisms as well, with one former patient recently highlighting the pressure on staff and beds and the high rate of suicides among patients who had been discharged.
There is also an ongoing investigation by police into the death of young Co Armagh man Seán Boyle in the unit in 2020.
The trust is part of the regional Towards Zero Suicide collaborative which aims to identify and respond to patients at risk of suicide as quickly as possible.
A risk assessment and management plan is undertaken for every patient admitted to Bluestone, and this is completed and updated within the community mental health teams.
Joe says that while it is impossible to completely eradicate the risk of suicide among the general public, there are ways to reduce it.
He points out that people who attempt suicide usually do it because of two things – a loss of hope and a feeling of being a burden.
“Suicide itself can be quite impulsive,” he explains. “There was a documentary about the Golden Gate Bridge in San Francisco, which hundreds of people have jumped from.
“Only five per cent who jumped survived and all of them said they regretted the decision immediately after they let go. One person said if he had had the intervention to stop and think, he probably wouldn’t have let go.
“What we learn from that is that those wee moments are really, really essential. Being able to have a conversation – to listen to the person, hear them and see them, and then work in collaboration with them to look at alternatives, while acknowledging their pain and their reality, to see their strengths and identify the support around them, that is so important.”
Lead nurse, Jennie Lee Sims, who lives in Katesbridge and “absolutely loves” her job, points out that all patients get a therapeutic one-to-one meeting every day and an opportunity to have that all-important conversation.

Another tool patients can use are ‘calm cards’ – a card which has been devised for each patient in consultation with them.
Says Jennie: “Rather than go to medication first, you go to your calm card. We have seen a massive reduction in the use of medication because of the use of our tranquillity room and calm cards – it might be a cup of tea, a phone call home or a walk outside.”
And one staff nurse, Nathan Weir, is proof of how the right intervention can transform lives.
Nathan, who has lived experience of mental ill health, has made it to the final of the NI Nurse of the Year awards, much to the delight of his colleagues, with the winners set to be announced this month.
Joe is a firm believer in the need to keep building sustainable voluntary and community resources in people’s own areas.
“I grew up in west Belfast during the Troubles – the boundaries of your street and area were your reality. It could be completely chaotic and unhealthy but it was your reality,” he says.
“Do we get caught up in that with no resources, no hope, no peer support? That just perpetuates that type of cycle.
“The 18-30-year old age group is the demographic that leans towards crisis admissions – they need somewhere to call into, like the Well-Bean Café in Newry, where there are trained people who can listen and where they can go in and meet their peers.”
While it has been 18 months of change, there is more planned for the future.
A new logo has been designed – a blue orchid symbolising hope and resilience – and the plans for a best standard dementia patient ward are currently with the Department of Health, with high hopes it will be approved and built within the next 18 months.
More staff are in the process of being recruited and the unit is currently going through an accreditation process with the Royal College of Psychiatry for its three general psychiatry wards and if successful, will be the first hospital to achieve the accreditation in Northern Ireland.
“It’s an assurance that what we are doing here every day is gold standard,” adds Joe.
“We are definitely on a journey and there has been so much achieved in such a short space of time, but that’s down to the strength of the team making it a centre of therapeutic excellence.”



